For Providers
We understand that you want more time to deliver high quality care to patients, and to spend less time navigating the changing healthcare landscape. The Chesapeake IPA (CIPA) is organized to make sure you can do that--and lead the market. Our strength is in numbers. When you participate in CIPA, you have access to resources and expertise that will improve your practice and patient outcomes and give you greater opportunities to do what you love – practice the art of medicine. CIPA awards providers a chance to engage in programs such as direct contracts with employers, the Direct Contracting Model, and the Medicare Shared Savings Program.
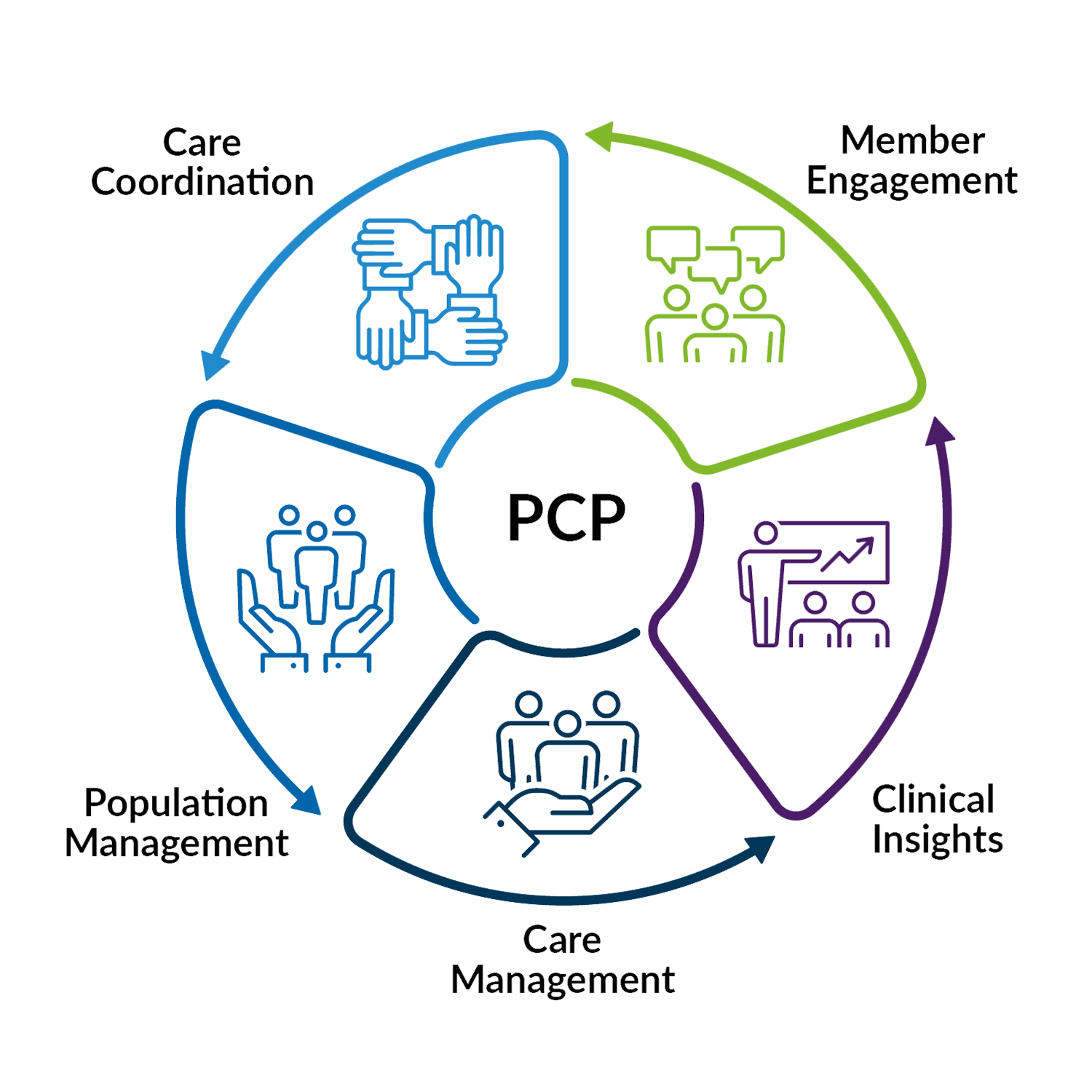
Let us support you in delivering high-quality care, improving the health of your patients, and lowering healthcare costs. Since we are provider-led, we live and understand the challenges of healthcare. CIPA reinforces your best efforts in value-based care programs by providing a framework for care coordination and new resources, including the most up-to-date technology, to close gaps in quality and care for patients. We work closely with practices to achieve their goals and desired outcomes.
Our Strategy
Through Collaborative Health Systems’ engagement with CIPA, we offer our participating practices:
- HealthyImpact 360, a customized population health management software platform where providers, care managers and patients collaborate more effectively for improved care and lower costs. HI360 integrates seamlessly into your practice EMR.
- Ignite, a fully HIPAA-compliant, web browser-based telehealth platform that provides virtual office visits for your patients.
- Consultative Services from a dedicated local team who assist practices with training on quality metrics, patient engagement, and managing high-risk patients.
- A Care Coordination Program to facilitate post-discharge transitions of care and reduce unnecessary hospital readmissions/emergency room visits.
- Reporting and analytics that provide your practices with insights into patient cost, utilization, completion of quality metrics, claims data, care gaps, and more.
- Assistance in achieving financial incentives available in Medicare Fee-For-Service arrangements and commercial health plans.
- The opportunity to join other Maryland providers in value-based programs such as Accountable Care Organizations and the Maryland Primary Care Program.